The fear of monkeypox
Posted by Doris Obinna | 7 years ago | 3,379 times

Like some years ago, when the dreaded Ebola reared its ugly head in Nigeria, anxiety, fears and panic have spread across the country, following the discovery of monkeypox in the country.
Many people have been confirmed dead, while scores have been isolated or quarantined in hospitals for contracting monkeypox.
Incidentally, this is the first time most Nigerians are hearing of monkeypox. This makes pertinent the question: What is monkeypox?
Monkeypox is an infectious disease caused by an orthopox virus. Orthopox viruses are a genus of viruses that include the disease agents that cause human smallpox, cowpox, and camel pox as well as monkeypox.
The monkey pox virus was first seen in monkeys. However, it could also be found in bush animals, such as rats (Gambia), squirrels, antelopes, striped mice, dormice and primates. Doubts persist on the natural history of the virus, as further studies continues to identify the exact reservoir of the monkeypox virus and how it is maintained in nature.
According to World Health Organisation (WHO), monkeypox was first discovered in 1958 when two outbreaks of a pox-like disease occurred in colonies of monkeys kept for research, hence the name ‘monkeypox.’ The first human case of monkeypox was recorded in 1970 in the Democratic Republic of Congo during a period of intensified effort to eliminate smallpox. Since then, monkeypox has been reported in humans in other central and western African countries.
The disease, so far, has been classified as a zoonosis, which means that it is a disease of animals that can be transmitted to humans under natural conditions. The first case of monkeypox reported in humans involved contact between humans and animals in the African rain forest.
The outbreak that made headlines in the United States in June 2003, however, involved animals purchased as pets from pet stores. It is not known, as of late 2003, whether other wild or domestic animals could contract monkeypox.
Nigeria on red list
The dreaded monkeypox virus has now paid Nigeria a visit. Many states have so far confirmed outbreak of the communicable disease, as earlier reported by the Ministry of Health. Bayelsa, the first state to be visited by the virus, is yet to come to terms with the reality of it.
The first case was reported in Agbura, a rural settlement in Yenagoa. It was gathered that the victim had killed and eaten a monkey with members of his household and neighbours, who later showed symptoms of the virus. At present, the state is tracking about 50 other persons who came in contact with persons already infected.
A medical doctor and 13 persons who came down with the monkeypox had been quarantined in an isolation centre at the Niger Delta University Teaching Hospital (NDUTH), Okolobiri, in Yenagoa Local Government Area of the state.
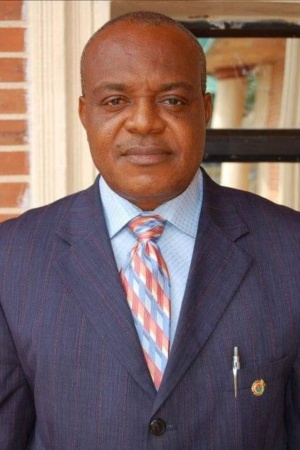
The Minister of Health, Prof. Isaac Adewole, had, during a briefing, said the health facilities in Bayelsa State had been placed at alert, with patients suspected of having monkeypox quarantined. He said monkeypox was a viral illness caused by a group of viruses that included chickenpox and smallpox.
“Investigation is still on-going and our partners are working with us on this reported outbreak, while the Nigeria Centre for Disease Control (NCDC) team in Bayelsa State would give support,” the minister assured.
Although Adewole said monkeypox could not be confirmed until laboratory investigations by WHO referral laboratory in Dakar, Senegal, he gave assurance that the disease was milder and had no record of mortality.
There is also red alert over the disease in Rivers, Lagos, Ekiti, Cross River and Akwa Ibom states.
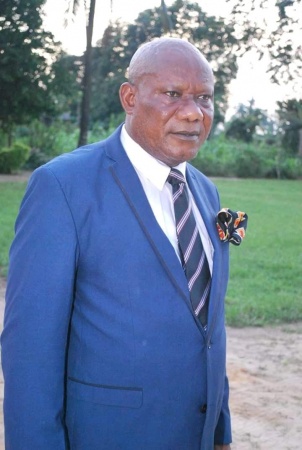
The Commissioner of Health in Rivers State, Princewill Chike, confirmed that three cases had been reported in the state. According to him, one was from the Rumuorlumeni area of the state, while another was a 13-year-old boy at Eneka.
“We discovered they took the boy to a native doctor. The parents thought they could handle it the native way,” the commissioner said.
How monkeypox could be contracted
Experts say infection of index cases results from direct contact with the blood, bodily fluids or cutaneous or mucosal lesions of infected animals.
In Africa, human infections have been documented through the handling of infected monkeys, Gambian giant rats and squirrels, with rodents being the major reservoir of the virus. Eating inadequately cooked meat of infected animals is a possible risk factor.
There is also human-to-human transmission, which results from close contact with infected person’s respiratory tract secretions, skin lesions or objects recently contaminated by patient’s fluids or lesion materials.
Transmission occurs primarily via droplet respiratory particles usually requiring prolonged face-to-face contact, which puts household members of active cases at greater risk of infection. Transmission can also occur by inoculation or via the placenta (congenital monkeypox).
In recent animal studies of the prairie dog-human monkeypox model, two distinct clades of the virus were identified – the Congo Basin and the West African clades – with the former found to be more virulent.
Signs and symptoms
Prof Adewole said the symptoms include headache, fever, back pain and, in advanced cases, rashes bigger than those caused by chickenpox. He urged anyone with symptoms of monkeypox to immediately report to the nearest health facility, while health workers were advised to maintain a high index of suspicion and observe safety percussion.
A recent study, however, noted that the incubation period (interval from infection to onset of symptoms) of monkeypox is usually from six to 16 days, but can range from five to 21 days. The infection can be divided into two periods. The first is the invasion period (0-5 days) characterised by fever, intense headache, lymphadenopathy (swelling of the lymph node), back pain, myalgia (muscle ache) and an intense asthenia (lack of energy).
The second stage is the skin eruption period (within 1-3 days after appearance of fever), where the various stages of the rash appears, often beginning on the face and then spreading elsewhere on the body. The face (in 95 per cent of cases), and palms of the hands and soles of the feet (75 per cent) are most affected. Evolution of the rash from maculopapules (lesions with a flat bases) to vesicles (small fluid-filled blisters), pustules, followed by crusts, occurs in approximately 10 days. Three weeks might be necessary before the complete disappearance of the crusts.
The number of the lesions varies from a few to several thousands, affecting oral mucous membranes (in 70 per cent of cases), genitalia (30 per cent), and conjunctivae (eyelid) (20 per cent), as well as the cornea (eyeball). Some patients develop severe lymphadenopathy (swollen lymph nodes) before the appearance of the rash, which is a distinctive feature of monkeypox compared to other similar diseases.
Monkeypox is usually a self-limited disease with the symptoms lasting from 14 to 21 days. Severe cases occur more commonly among children and are related to the extent of virus exposure, patient’s health status and severity of complications. People living in or near the forested areas may have indirect or low-level exposure to infected animals, possibly leading to subclinical (asymptomatic) infection.
The case fatality has varied widely between epidemics, but has been less than 10 per cent in documented events, mostly among young children. In general, younger age-groups appear to be more susceptible to monkeypox.
Diagnosing monkeypox
Experts proposed that the differential diagnoses that must be considered include other rash illnesses, such as, smallpox, chickenpox, measles, bacterial skin infections, scabies, syphilis, and medication-associated allergies.Lymphadenopathy during the prodromal stage of illness can be a clinical feature to distinguish it from smallpox.
Prevention
Experts advocates restriction of animal trade or ban in movement of small African mammals and monkeys as a way of slowing down the expansion of the monkeypox virus outside Africa. They say potentially infected animals should be isolated from other animals and placed into immediate quarantine. Also, any animals that might have come into contact with an infected animal should be quarantined, handled with standard precautions and observed for 30 days.
Treatment
There is no known treatment at present. However, outbreaks of monkeypox can be controlled. Smallpox vaccine, Cidofovir, ST-246, and vaccinia immune globulin (VIG) could be used to control the disease.
The Centre for Disease Control (CDC) recommends the following: A smallpox vaccination should be administered within two weeks of exposure to monkeypox. However, as they say, prevention is better than cure. It is better not to contract the disease. Towards this end, crowded places and infected people should be avoided as much as possible.
An expert advised: “During human monkeypox outbreaks, close contact with other patients is the most significant risk factor for monkeypox virus infection. In the absence of specific treatment or vaccine, the only way to reduce infection in people is by raising awareness of the risk factors and educating people about the measures they can take to reduce exposure to the virus. Surveillance measures and rapid identification of new cases is critical for outbreak containment.”
Readers Comments
comment(s)
No comments yet. Be the first to post comment.